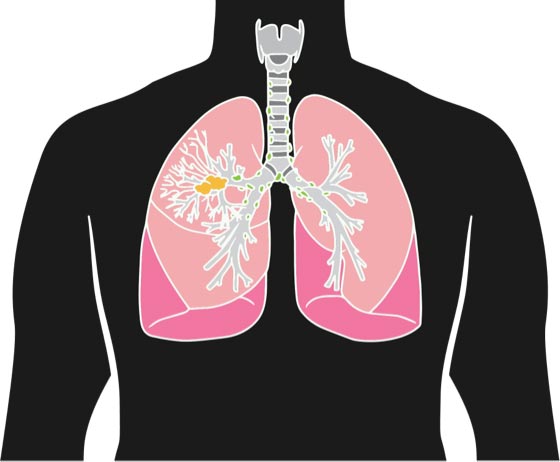
There are a number of symptoms you should look out for, including:
- coughing up blood
- a new or changed cough that doesn’t go away
- pain in their chest or shoulder
- being short of breath, or trouble breathing
- hoarse voice
- chest infection that won’t get better
- feeling very tired or weak
- not feeling hungry or losing weight without meaning to.
Anyone can get lung cancer, even people who have never smoked.
Having these symptoms may not mean you have cancer, but it’s important to check.
If you have any of these problems or are worried about any of these symptoms, yarn with your doctor, nurse or Aboriginal and/or Torres Strait Islander health worker.