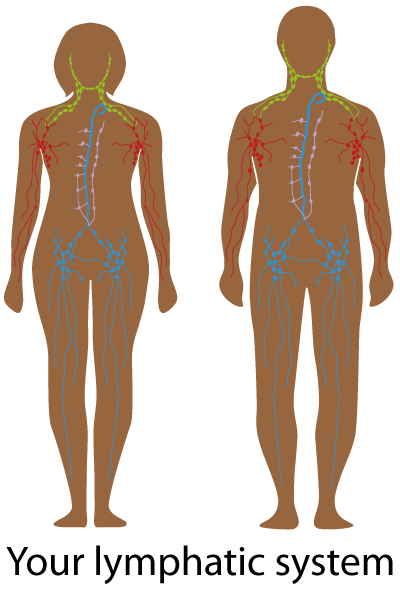
There are a number of symptoms to look out for, including:
- painless, swollen lumps around the neck, groin or under the arms
- feeling really tired
- night sweats
- fever
- itchy skin
- losing weight without meaning to
- not feeling hungry
- getting sick a lot
- bleeding or bruising easily
People and kids can also have swollen tummy, coughs and trouble breathing, headaches or skin changes like lumps or blotches.
Having these symptoms may not mean you have cancer, but it is important to check.
If you have any of these problems, or are worried about something else, yarn with your doctor, nurse or Aboriginal and/or Torres Strait Islander Health Worker.