There are a number of symptoms or changes you should look out for, including:
- bleeding from the vagina between periods
- bleeding from the vagina after menopause (the time when women stop having their periods)
- pain or bleeding during or after having sex
- having an unusual discharge or blood coming from your vagina
- having heavier or longer periods than normal
- feeling very tired
- unusual swelling in your legs
- leg or back pain.
Having these symptoms may not mean you have cancer, but it is important to check.
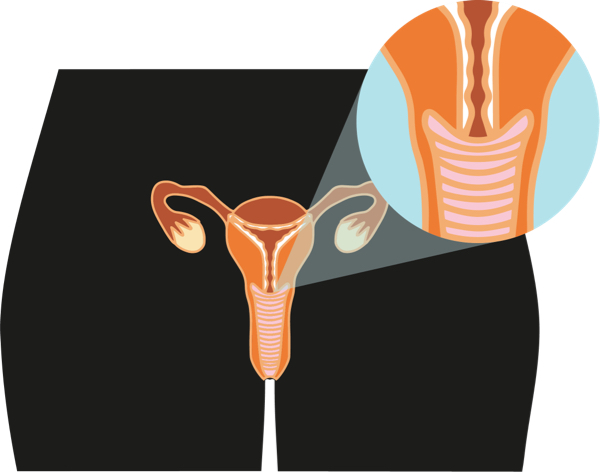
If you have unusual bleeding, discharge or pain, see your doctor, nurse or Aboriginal and/or Torres Strait Islander health worker. If you have bleeding that is unusual, you may be referred to a gynaecologist, who is a doctor that specialises in women’s health.
Sometimes when women find out they have cervical cancer, they may not have had any symptoms and never knew they had a problem.
If you have any concerns or are worried about something else, yarn with your doctor, nurse or Aboriginal and Torres Strait Islander health worker.